- Home
- Sailing Authors & Their Writings
- Dr Michael Cohen
- Solo Sailing
Solo Sailing and the Need for Sleep
by Dr Michael Cohen
Solo sailing has always been a major challenge whether or not the sailor is engaged in an athletic contest such as the OSTAR single-handed transatlantic race or simply sailing solo.
According to the collision regulations which govern all mariners (COLREGS) there must be a proper watch at all times. That is by nature inconsistent with sailing solo – a man or woman has to sleep, period; and as long as that is recognized we move on to the next point – how to maximize performance while dealing with the need to sleep. Basically, how to arrange our sleep to get enough to minimize a decline in performance and maximize maintaining a proper watch in order to avoid collision or running aground.2
Is there anything a solo sailor can do? Yes, the first thing is to identify your chronotype. Basically, are you a morning person (a 'lark'), an evening person (an 'owl') or an intermediate (sometimes call a 'hummingbird')?
It turns out that this is the first step in sleep management. A recent article in the publication Nature and Science of Sleep analyzed a number of strategies in sailors who participated in the Mini Transat La Boulangere a race across the Atlantic for 4,050 miles (6518km). The race is from the west coast of France to Martinique with one stop in the Canary Islands. There were 42 skippers who completed questionnaires about the quality of their sleep, their somnolence, and their chronotype.
Of the skippers 40% were larks, 60% were intermediates i.e. hummingbirds, but there were no 'owls'. So, it seems that most captains – at least those who partake of solo single handed sailing races – are not night owls. Larks were overrepresented (in the population it should be closer to 25%) and owls may actually be at a disadvantage in these type of endurance events.
Of the skippers who adopted a sleep management strategy most were of the intermediate hummingbird type rather than the lark type who didn’t seem to need to adopt a specific strategy.
What kind of strategies?
- Polyphasic sleep – breaking up the sleep into 2 or more segments or simply taking planned naps throughout the day and night (see below the case of Ellen MacArthur). Cultures with a 'siesta' are practicing polyphasic sleep although the siesta may be little more than a brief nap. Breaking up sleep into multiple naps has a tried-and-true tradition and has been a common approach for long distance solo sailors and it works.3
- 'Banking' sleep – that is, 'oversleeping' in the days and weeks before the race or extended period offshore. Obviously, this will only work for races or cruising of limited duration and it isn’t certain that it helps; but there is some evidence that it is effective in shift-workers.4
Napping should be done correctly, trying to awaken at the end of a REM period – so 20 minutes is a good starting point. That way you tend to awaken with less sleep inertia. If that works, try 80-90 minutes. Dr Claudio Stampi who is the director of Chronobiology Research Institute in Newton, Massachusetts discusses how to manipulate this in a Sail Magazine article 'Sleep and Seamanship'.5 He monitored Dame Ellen MacArthur during her 2000-2001 Vendee Globe non-stop 94-day singlehanded circumnavigation. Analysis of her sleep revealed that she…
- Averaged 5.7 hours of sleep per day. Her longest period of uninterrupted sleep was 2.7 hours. Her longest period of uninterrupted wakefulness was 18.5 hours. She averaged 9.4 naps per day, 72 percent of them in clusters of three or more. Her average nap was 36.6 minutes. MacArthur was 24 years old at the time, the youngest entrant ever in that gruelling race. She placed second.
Covid-19
Perhaps now, after the 2020 US election, we can all try to get some sleep! We’d better, as we are still dealing with Covid and probably will be for the next year. But wait, does Covid-19 effect our sleep? It certainly does and in fact some experts now refer to it as 'Coronasomnia'.
Covid has created a world of chronic insomniacs trying to deal with reduction in productivity, stress, shorter fuses, depression, hypertension, and a variety of other health problems. In addition to the financial stresses, days now lack social interaction as well as their previously normal daily rhythm. Kids are home and bedrooms are now serving as makeshift offices.
You should be aware that although light and darkness are important in regularizing our circadian rhythm (Zeitgebers in sleep lingo), so are our daily routines such as eating times, exercise, riding the train or the car commute, etc. All of these changes will tend to throw off our circadian rhythm.
Sleep researcher, Professor Tore Nielson director of the Dream and Nightmare Laboratory at the Universite de Montreal has documented how Covid has altered our dream world.1
One unexpected consequence of working from home is that sleep patterns change and the absence of sometimes long commutes to work has allowed an increase in sleep of an hour to 1 and ½ hours. Since REM sleep predominates toward the end of our sleep, the extra sleep ensures that dreaming (which occurs most prominently in REM sleep) is more likely to be recalled.
The subject matter of these dreams often reflects events in our lives so you can imagine that various infections become prominent themes. Deirdre Barrett of Harvard and editor of the Journal Dreaming initiated an online survey in March 2020 and there is apparently a Twitter account @CovidDreams.
The US Navy and Covid-19
Since 2017 the US Navy (The Naval Postgraduate School in particular) has been focused on sleep. It turns out we need good restful sleep to help protect us from Covid. At least it appears that way and the Navy is taking no chances. The Navy’s Crew Endurance Team has emphasized that in addition to the well-known best practices – social distancing, wearing a mask, and washing your hands – sleep is important to keep our immune system strong and resilient. The relationship between sleep and the immune system is complicated but there are now multiple studies over the last 15 years which have documented that sleep helps us create the cells and antibodies which fight off pathogens like bacteria and viruses.
This is particularly problematic for shift workers like sailors and medical personnel, who struggle to get sufficient sleep.
It is still early in the pandemic to expect hard science, but the issue of stress, workload, sleep loss and the effect on the immune system is very much on people’s minds. 6, 7I would expect that once the studies are completed that the combination of stress, prolonged shifts, rotating shifts, and sleep loss will be implicated – at least in part – in the loss of life in front line medical personnel.
The Masculinity Syndrome
American myths and stereotypes seem to persist forever!
One such problem is 'The Sleep-Deprived Masculinity Stereotype Syndrome,' as documented in a new paper in the Journal of the Association for Consumer Research.8
The syndrome is typified by the quote, "I’ll sleep when I’m dead".
Unfortunately, this syndrome is still present despite decades of research documenting how counter-productive it is.
Time's Up?
The American Academy of Sleep Medicine is calling for the elimination of daylight savings time (DST), supporting a switch to permanent standard time.

The proposal has been endorsed by 20 organizations including the National Safety Council, National PTA, World Sleep Society, American College of Occupational and Environmental Medicine, Society of Behavioural Sleep Medicine, and multiple state sleep societies.
The position paper cites evidence of an increased risk of cardiovascular events (heart attacks and strokes), mood disturbances, and motor vehicle accidents attributed to the annual 'spring forward' to daylight savings time.
Traffic fatalities increase by as much as 6% and adverse medical events by 18% in the few days following the time switch. The reason is that DST results in more darkness in the morning and more light in the evening, disrupting the body’s natural rhythm.9 If this doesn’t make immediate sense, I would recommend re-reading the chapter on sleep in Healthy Boating and Sailing!
A recent poster presented at the conference Sleep 2020 by researchers at the Mayo Clinic found a statistically significant increase in adverse medical events in the week after the annual time change in the spring. Something to think about when planning your next March operation!
Shit-For-Brains
I was hesitant to use this urban slang from my youth, but since it appears in The Cambridge Dictionary, admittedly as 'US offensive' – and since I’m a Philly boy at heart, I figured that gives me some degree of license!
So, we are all aware, or should be, of the importance of our microbiome in health and disease. But I confess, I had never imagined there was such a thing as the 'brain-gut microbiome axis' (BGMA). Who knew?
Researchers at the University of Missouri-Columbia were studying Obstructive Sleep Apnea (OSA). The study exposed mice to either room air or intermittent hypoxia (poor oxygen level) designed to mimic OSA. After 6 weeks they collected fecal material from the mice.
A third group was divided in two and was given a fecal transplant from the room-air-group or the hypoxic group. They found that the mice transplanted with the intermittent hypoxic fecal material slept longer and more often suggesting increased sleepiness10.
This axis works both ways as sleep fragmentation increases blood pressure and is associated with alteration in the gut microbiome and fecal metabolome in rats.
Contrary to the initial hypothesis the changes in the gut microbiome took a week to show unfavorable changes including an imbalance in the bacterial types as well as an increase in bacteria associated with inflammation. And once the sleep disruption stopped, the microbiome did not revert to 'normal' immediately. The BGMA is one complex system11.
The Glymphatic System
Despite centuries of careful neuroanatomy dissection and study, it wasn’t until 2012 that Dr Maiken Nedergaard (University of Rochester Medical Center) discovered a most important piece of plumbing of the brain – the glymphatic system.
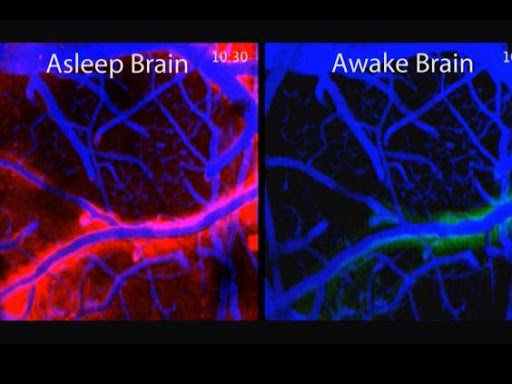
The glymphatic system follows the blood vessels and pumps cerebrospinal fluid (CSF) through the brain tissue (see the 'Asleep Brain' figure above – don’t pay any attention to the color just the amount of flow along the vessel in the 'asleep brain' versus the 'awake brain'). It basically washes away waste while we sleep (and as I mentioned previously in the book, it seems to work best if you sleep on either side rather than on your back or chest!).
Since it only functions during the normal sleep period (and not even during anaesthesia), people who rely on cat naps or who work night shift or shift work may be at increased risk of not clearing this waste (including amyloid?) from their nervous system.
Whether this is a risk factor for lifelong solo cruisers with poor overall sleep time, only time will tell.
It also turns out that the brain cells known as astrocytes (always considered supporting players unlike the neurons which were considered the stars of the show) – may control the flow of CSF through the brain and into the glymphatic system.
Since the glymphatic system empties into the lymph nodes in the neck and because the lymph nodes are important in the regulation of the immune system, this research suggests that the CSF clearance may represent a 'fluid clock' that in a sense 'wakes up' the body’s infection fighting capabilities for the upcoming day!12
Sleep Medicine
Probably no group is more concerned with performance readiness than the US Marines. The Operations Research Department (Naval Postgraduate School) studied the effects of sleep on both cognitive and physiologic performance after 2 hours after wakeup.

Short sleep duration and elevated sleepiness were associated with worse (higher) completion times in the obstacle course and elevated sleepiness was also associated with lower cognitive throughput (number of correct responses per minute). The results suggest that sleep-deprived marines experience poorer executive decision making.13
The US Navy’s Crew Endurance Program has a number of current projects including:
- The development of circadian based watchstanding schedules assessing the watchbills (naval term for watchkeeping schedules) on multiple types of ships during different phases of readiness 'to provide a thorough comparison of various watchstanding schedules. In addition, it will identify problems and potential solutions for the effective implementation of circadian watchbills'. The navy is certifying the development of better, more circadian-based watchkeeping – ship by ship. It is not an easy proposition.
- Reducing sleep inertia. As I discussed in the chapter on sleep, there is a period of time after awakening (usually 15-60 minutes) during which there is drowsiness and some disorientation associated with impaired sensory and motor acuity, impaired attentiveness, mental ability and subjective fatigue. This is in the absence of any sleep deprivation. The navy is studying countermeasures such as stimulating multiple sensory modalities including visual, auditory, somatosensory, and olfactory! Right now, all we have is blue light and a cup of Joe (which takes up to 30-45 minutes to get to peak concentration).
- There are also attempts in the Navy to improve the sleep experience by using thicker, weighted curtains to improve the sound and light environment for the sailors and hopefully promote better sleep. The US Navy is looking at anything and everything to improve the sleep of their sailors.
Insomnia
There are a number of new agents which have been approved by the US FDA for use in sleep disorders – the first two are mainly for people diagnosed with Narcolepsy or Sleep Apnea syndrome.

Big pharma (if true to form) will count on these being used 'off label' for people who need some pep during the day. The third is for insomnia and is meant to be used at night. Almost certainly you don’t need any of these. I include them because they are new and they have great brand names, especially 'Dayvigo' although I would not necessarily have chosen it for a medication to help put you to sleep!
1. Pitolisant (Wakix) which increases histamine in the brain and wakes you up! [that’s right, histamine wakes you up which is why an 'anti-histamine' like Benadryl may cause sedation]
2. Solriamfetol (Sunosi) which blocks the re-uptake of dopamine and norepinephrine (similar to amphetamine) and allows more of them to circulate and keep you awake.
3. Lemborexant (Dayvigo) which blocks the neurotransmitter 'orexin' which wakes you up. Therefore, is to be used at night to help sleep – especially for older adults.
HOWEVER, the pendulum has clearly shifted in the sleep medicine field, away from pharmaceuticals toward behavioural treatment as first line therapy for insomnia. Of course, that doesn’t stop big pharma in the US from pushing drug treatment.
There were two recent studies of Cognitive Behavioural Therapy for Insomnia (CBT-I). One was from Australia and involved 455 'real world' insomnia patients with or without symptoms of depression, anxiety, and stress. They found marked improvement in sleep – a similar amount between patients without and with depression, anxiety, or stress.14
A recent Norwegian study evaluated unguided online CBT therapy for chronic insomnia – CBT-I. The aim was to see whether fully automated internet-delivered CBT-I was effective over the long haul, e.g. at 18 months. It turns out that it was, and it was comparable to in-person CBT-I. There was some reduction at 18 months but as the authors point out there were no booster sessions. They opined that had there been, the results at 18 months would have been even better.15
These two studies, as well as numerous others point to behavioural therapy, including CBT-I, meditation, mindfulness-based stress reduction, relaxation therapy etc. – and not drugs – as the first line of defence for insomnia patients.
1 Scientific American October 2020
2 In order to understand this aspect of the blog you should read Chapter 12 of Healthy Boating and Sailing. If we are this close to having self-driving vehicles prowling our streets, I would hope that someone is working on a much simpler system for the nautical community. Not just for singlehanded or shorthanded sailors (and the Navies around the world) but for the maritime industry as well).
3 Monphasic sleep (7-9 hours in one block at night) seems to be a relatively new phenomenon – dominant since the industrial revolution. Prior to that biphasic or polyphasic sleep patterns appear to have been the norm.
4 Patterson, Ghen, et al. Does evidence support “banking/extending sleep” by shift workers?… Sleep Health 5 (2019) 359-369
5 Charles Thraser, Sleep and Seamanship, Sail Magazine May 2019
6 Ferini-Strambi et al. Covid-19 and Sleep in Medical Staff: Reflections, Clinical Evidences, and Perspectives, Curr Treat Options Neurol. 2020 22:29
7 Herrero San Martin et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic, Sleep Medicine online 17 August 2020
8 The Journal of the Association for Consumer Research, University of Chicago Press Journals, September 2020
9 www.sciencedaily.com/releases/2020/08/200827150951.htm
10 Badran et al., Fecal microbiota transplantation form mice exposed to chronic intermittent hypoxia elicits sleep disturbance in naïve mice, Experimental Neurology, 2020; 334: 113439
11 Maki, et al. Physiological Genomics, 2020:52 (7) 280
12 Hablitz, et al. Circadian control of brain glymphatic and lymphatic fluid flow. Nature Communications, 202; 11(1)
13 Shattuck, Shattuck, Matsangas, Combat Effectiveness and Sleep Patterns in the US Marines
14 Sweetman, et al, Do symptoms of depression, anxiety or stress impair the effectiveness of cognitive behavioral therapy, Sleep Medicine 75; 401-410, 2020
15 Vedaa et al. Long-Term Effects of an Unguided
Online Cognitive Behavioral Therapy for Chronic Insomnia. J. of Clinical Sleep
Medicine 15: 1 101-110
Recent Articles
-
Island Packet 40 Review: Specs, Performance & Cruising Analysis
Feb 09, 26 05:05 AM
An in-depth review of the Island Packet 40 sailboat. Explore technical specifications, design ratios, and real-world cruising performance for this legendary blue-water cruiser. -
Beneteau Oceanis 331 Clipper Review: Specs, Performance & Ratios
Feb 04, 26 07:25 PM
A comprehensive review of the Beneteau Oceanis 331 Clipper sailboat. We analyse design ratios, interior layout, and performance for prospective cruising owners. -
Self-Tacking Headsails: Track Systems vs Hoyt Jib Booms
Feb 03, 26 06:26 AM
Master the mechanics of self-tacking headsails. We compare traditional club-footed rigs, curved tracks, and the superior Hoyt Jib Boom for offshore sailing.